A Clinical Trial from the inside
A Clinical Trial from the inside
Julia Greenland
It’s an exciting time in the Williams-Gray Parkinson’s disease research group! We are finally opening our clinical trial of azathioprine in PD (AZA-PD). It’s been a long road, which has involved lots of delays (to say nothing of the pandemic), but yesterday I sent out the first 8 invitation letters. I now have my fingers crossed, hoping for some eager participants!
The group has been researching the immune system in PD for a number of years now, and has found several clues that imply it is involved in causing PD to progress. And even that it may help to answer the question of why some people might get Parkinson’s disease in the first place. Our work fits in with what people all round the world are also finding; that the immune system seems unusually active and primed to respond to some of the disease-related changes, such as the accumulation of alpha-synuclein in dopamine producing cells in the brain. Despite the weight of evidence pointing towards its involvement, the only way to tell for sure if changing the immune system can slow down PD is by running a clinical trial and testing an immune medication as a treatment in patients. This is not something that can be proved with experiments in the lab. The medication that Caroline (Dr Williams-Gray) chose is one that is well known to doctors. It is called azathioprine and dampens down the immune system. Although it has side effects (there isn’t a tablet without them), we know what the problems are, how to spot them early and what to do to sort them out.

My involvement in this trial started in late 2017. I had just had a baby and come back to work as a neurology registrar in Addenbrookes hospital in Cambridge. As part of my training to become a neurology consultant, I was planning on embarking on a PhD. I’d previously done a small amount of research in PD in Newcastle whilst I was a medical student, and I’d emailed Prof Roger Barker looking for a clinical project that I could get involved in. He put me in touch with Caroline. It feels like I’ve had a long road to get here, but Caroline’s is much longer. By the time I came on-board she had come up with the concept, designed the trial and successfully secured funding through the Centre for Parkinson’s Plus. (Naively) at that point it felt that the majority of the large hurdles were cleared. I started at the John van Geest Centre for Brain Repair in January 2018, working on writing the protocol and associated documents that accompany the running of a clinical trial, and preparing the application for the Research Ethics Committee. We thought we would be recruiting patients by the end of that year…
It’s year three, another baby and one pandemic later. But we are here. On the brink of welcoming our first participants to AZA-PD. (Fingers crossed for no further hiccups!).
Today I confirmed our first official participant! It’s taken longer than I imagined to get underway. So far, I’ve sent invitations to 40 people, and 11 have signed up for screening to determine if they’re eligible. I have to follow a process of sending information sheets out to people who have consented through our research clinic, then waiting two weeks, before following up with a phone call. I can then book people who are interested in for a “screening visit”. This is where I meet people face-to-face and we go through checks to see if they formally meet criteria to enter the trial. As you can imagine, we have to be very strict with these checks, as our approval by the research ethics committee relies on us following the pre-written protocol word for word.
When I’m ringing people, I almost miss lockdown, when you could be sure that people would be at home and would answer their phone! But once I get through, everyone has been so open to talking with me. There’s been a whole range of responses including “when can I sign up!” which always makes me really excited. And despite planning this for the last three years, I’ve been asked questions I hadn’t thought of. It’s good to be kept on your toes.
One of the hardest things that I’ve found is finding the balance between optimism and realism when talking to potential participants. I’ve been trying very hard not to promise things that we can’t guarantee, but I had a colleague sit in whilst I was talking to a potential participant the other day, and he commented that I could be a little more positive! It’s true, we don’t know for sure that azathioprine is going to slow Parkinson’s disease down (which of course is why we’re doing the trial), but there’s lots of evidence to suggest that it will. We are asking people to give up a lot of their time to be part of their trial, and I’m relying on a huge amount of altruism on the part of our patients. However, there is a half chance that they will be getting active treatment and will get a personal benefit. Plus I’m planning to make the visits as enjoyable as possible!
My challenge today was trying to coordinate getting my first prospective participant into the scanner for a PET/MRI before they enter the trial. I had to confirm that they were eligible and had passed screening by getting the results of a blood test- TPMT, which had been shipped to Birmingham for analysis. Foolishly, I thought I knew which hospital lab it had got sent to. I ended up ringing three, before getting to the right one, and was then on hold for the best part of an hour. But I got the result! This was brilliant, because it meant that I made the deadline to confirm the PET/MRI appointment for next week. We’re on a really strict timeline to make sure I follow everything as per the pre-defined protocol. What was most frustrating was the fact that the blood result had been ready for a week, and only took 2 days to process. It seems the only delay is one lab emailing another one.
The next exciting milestone is the first “baseline” trial visit for this participant, happening in two weeks’ time. This is where they will receive a pot of the trial medication (placebo or azathioprine)…
21/6/21
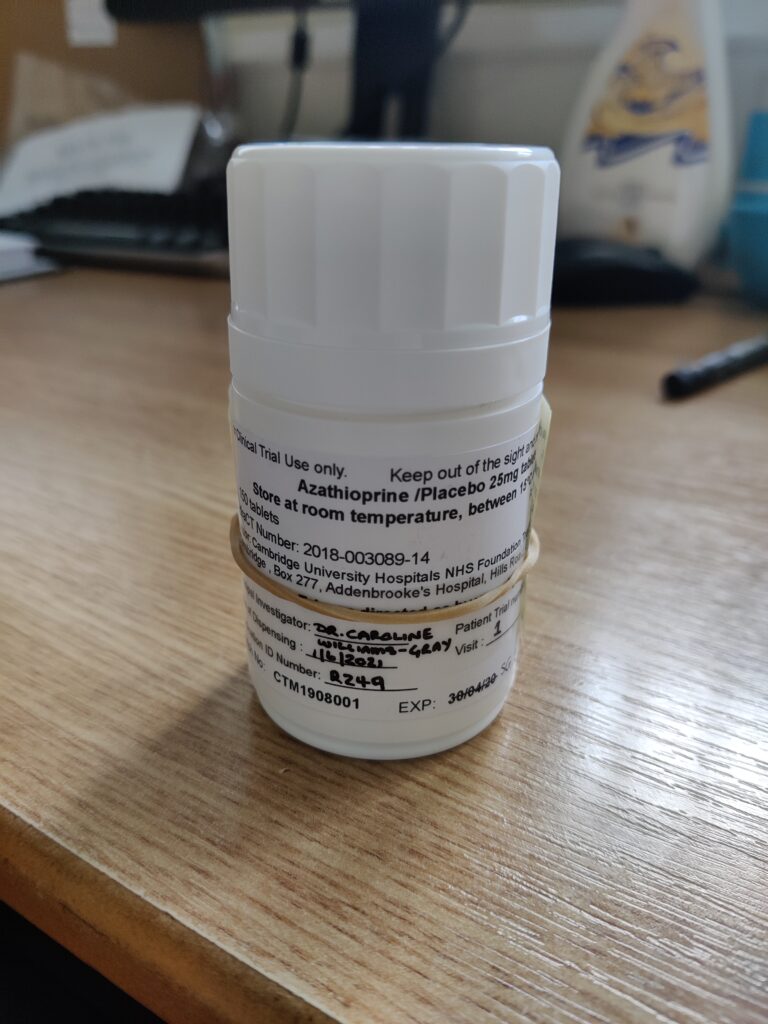
We are now properly underway; I have two people taking trial medication! In fact, I think picking up the first pot of tablets from pharmacy was the most exciting point to date. I suppose that it hadn’t felt entirely real until then. But there was no escaping the fact that I was starting a patient on a new treatment. I particularly enjoyed the label which said “azathioprine/placebo”, because of course, neither I nor the participants have any idea which of the two they will be taking.
One of the things that I’ve been asked the most often from patients who are signing up to participate is whether they’ll be able to keep taking the medication after the end of the trial if it’s working for them. The first difficulty is that, until we have the results from all of the participants, we won’t know whether it’s been effective. We’re not expecting that azathioprine will make people feel better from their Parkinson’s on a day-to-day basis. It’s not like levodopa treatment, which helps the stiffness and slowness that comes with the disease. We’re hoping that it’s going to have a different role, for which there is no treatment currently. We hope that it will slow down the underlying progression of the disease, or even stop it in its tracks. That means that the people who are taking the treatment won’t necessarily feel any better, and probably wouldn’t know personally if it has worked. We expect that instead, they will be in a much better place than they would have been if they hadn’t had treatment. And the only way that we can tell that is to compare how they have done with the people who had been taking placebo.
Of course, the other issue is that NICE (National Institute for Health and Care Excellence) will need to approve a new treatment for Parkinson’s disease before it can be used in practice. And they are likely to need a larger “phase III” trial before they can do this. So, in short, this is the first (necessary) step on a new treatment approach for PD. Unfortunately, the best that I can offer my patients currently is to give them this opportunity for the potential of a year’s worth of treatment with azathioprine. But what they are doing is giving hope for other patients in the future.
Another hurdle that we’ve recently cleared is our first “monitoring” by the Clinical Trials Unit. Of course, this is a really important and necessary thing to happen, where an independent expert in running trials inspects us and checks that everything is happening as it should be. But it’s nerve racking, particularly when Caroline and I are putting so much into making sure things are going smoothly. In fact, I spent several hours prior to the visit with all of the lever arch files spread around me making sure that I had dotted all of the i’s and crossed the t’s. And thankfully, the monitoring went well. A few minor paperwork issues, but nothing more. We were even complimented on our documentation, which was surprising, as it definitely doesn’t come naturally to me!
So now that the trial is underway, my job is to keep the momentum going. To be successful, we have to recruit 60 people over the next 12 months. There won’t be any let up- I need a steady stream of people coming through; at least one new participant per week. But we have the perfect set up and have been met with so much enthusiasm so far, I’m sure we’ll have no problems.

